|
Recommended Products
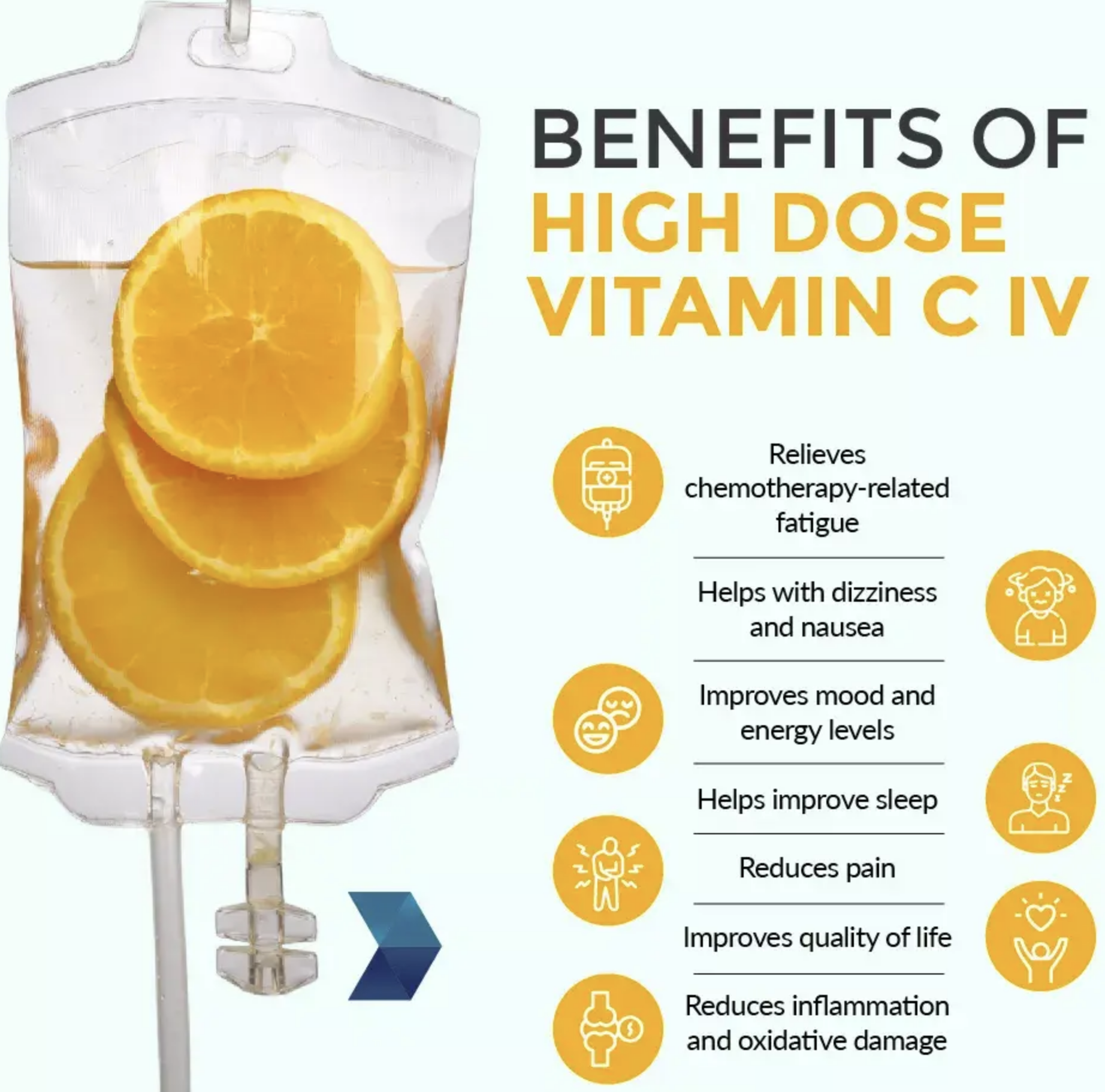
Vitamin C IV therapy has become increasingly popular over the last few years. A variety of micronutrient cocktails have been created with the goal to help support everything from dehydration and hangover to immune function and treating cancer.
About this item
500 Grams, MSM (Methylsulfonylmethane) Powder
Guaranteed 100% Pure. No Fillers or Additives.
Lab Tested and Verified.
Import Origin: USA.
Improves flexibility, Detoxifies the body, Strengthens hair and nails, Accelerates energy
|
|
CANCER - ALL YOU NEED TO KNOW CERVICAL CANCER – PATIENT INFORMATION
Cervical cancer is a common cancer of the female reproductive system. Cervix is the lower, narrow end of the uterus (womb) that connects the uterus to the vagina (birth canal). Although the cervix is part of the uterus, uterine cancer is diagnosed and treated differently. As per global statistics in 2022, cervical cancer is the 8th most common cancer in the world and the maximum number of cases is from Asia. Some people develop cervical cancer due to certain risk factors, whereas, some even develop cervical cancer with no known risk factors.
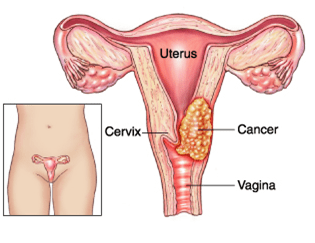 Cervical cancer starts as areas of abnormal, microscopic cells on the surface of the cervix [cervical dysplasia] due to changes in the DNA [mutations] of those cells. If left untreated, cervical dysplasia may progress to cervical cancer.
Almost all cervical cancer cases (99%) are linked to infection with high-risk human papillomaviruses (HPV), an extremely common virus transmitted through sexual contact. Most sexually active people have or had HPV at one point and mostly the immune system gets rid of HPV from the body. In other people, the virus causes long-term cell changes that develop into cancer, usually over decades after the initial infection. Among the many strains of HPV, some are more likely to lead to cancer [eg: HPV- 16 and 18]. Vaccines are also available to prevent HPV infections.
The investigations are done for staging the disease. The treatment plan is exclusively tailored for each patient, based on the stage and general health of the patient as per the treatment guidelines.
If the cancer has spread beyond the cervix [locally advanced], surgery is not performed, instead other treatment options are offered. The other treatment options are :
- Radiotherapy,
- Chemoradiation [where radiation and chemotherapy is given concurrently -i.e., during the same time period] &
- Systemic therapy [chemotherapy, targeted therapy, immunotherapy]
Radiotherapy uses high-energy waves similar to x-rays to kill cancer cells.
Common side effects during the 5 to 6 weeks of external radiation
[ External Beam Radiotherapy-EBRT]
- Fatigue
- Skin redness and irritation
- Diarrhea
- Nausea
- Frequent or painful urination
As part of chemoradiation, there are typically 5 radiation sessions [fractions] per week for 5 to 6 weeks. Chemotherapy is typically given once weekly during this time.
After completion of the radiation or chemoradiation, most patients require internal radiation therapy [Brachytherapy] – usually in the final week or right after completing EBRT. It involves treatment with radioactive material placed inside the body with the help of instruments [brachytherapy applicators] placed in the cervix, uterus and vagina.
The total treatment period with both types of radiation therapy would be around 7 to 8 weeks.
Supportive care refers to a range of care and resources such as Hospice care, access to pain specialists, and emotional and spiritual support, often needed by patients.
GENERAL DETAILS OF THERAPY
Chemoradiation – where radiation and chemotherapy is given concurrently i.e., during the same time period] and systemic therapy [chemotherapy, targeted therapy, immunotherapy]
Radiation therapy uses high-energy waves similar to x-rays to kill cancer cells. In external beam radiation therapy (EBRT), a large machine aims radiation at the cancer site. The radiation passes through skin and other tissue to reach the tumor and nearby lymph nodes. Common side effects during the 5 to 6 weeks of external radiation [ EBRT] include fatigue, skin redness and irritation, diarrhea, nausea, and frequent or painful urination. Most of these side effects develop gradually.
Types of Cervical Cancer 1.Squamous Cell Carcinoma:
2.Adenocarcinoma:
3.Other Rare Types:
Treatment Options Treatment depends on the cancer’s type, stage, and the patient’s overall health and preferences. 1. Early-Stage Cervical Cancer
•Radiation Therapy:
•Chemotherapy:
2. Locally Advanced Cervical Cancer
•Brachytherapy: Internal radiation therapy targeting the cervix. 3. Advanced or Metastatic Cervical Cancer Chemotherapy: Drugs such as cisplatin, carboplatin, or paclitaxel. •Targeted Therapy: Drugs like bevacizumab (Avastin), which inhibits blood vessel growth in tumors. •Immunotherapy: Agents like pembrolizumab (Keytruda) for advanced cancers with specific biomarkers (e.g., PD-L1). Follow-Up Care: Regular pelvic exams and imaging (e.g., CT, MRI, or PET scans) to monitor recurrence. Prevention: HPV Vaccination: Protects against the human papillomavirus (HPV), a major cause of cervical cancer. Routine Screening:
Timely diagnosis and treatment significantly improve outcomes. Discussing options with a multidisciplinary team is essential for personalized care. For further guidance, consult reputable oncology resources like Cancer.gov or the American Cancer Society. Cervical cancer treatment breakthrough cuts risk of death by 40%
In this study, 250 women with cervical cancer received the new treatment - an intensive six-week course of carboplatin and paclitaxel chemotherapy, followed by the "usual" treatment of radiotherapy plus weekly cisplatin and brachytherapy, known as chemoradiation.
Another 250 women - the control group - received only the usual chemoradiation. Five years later, 80% of those who had received the new treatment were alive and 73% had not seen their cancer return or spread. In comparison in the "usual" treatment group, 72% were alive and 64% had not seen their cancer return or spread. Dr Mary McCormack, lead investigator of the trial from UCL Cancer Institute and UCLH, said: "Our trial shows that this short course of additional chemotherapy delivered immediately before the standard CRT can reduce the risk of the cancer returning or death by 35%. "This is the biggest improvement in outcome in this disease in over 20 years." |
|
CANCER - ALL YOU NEED TO KNOW |
Oncology (Cancer) & Nuclear Medicine
This site has been developed for Cancer Patients & their Relatives under the 'Right of information for Patients'.
You may translate this page by clicking on the 'Select Language' - Top Left.